H E A L T H I E R H E A L T H C A R E
(Development ongoing)
(ABSTRACT)
"Healthcare is complicated" say Bernie Sanders and Donald Trump. But that is precisely the problem—It shouldn't be.
The experts have advised us that the complexity of our healthcare system is the greatest barrier to reform and we assume that the solution must be equally complex and overwhelmingly expensive.
But exactly what complexity are they all talking about? Healthcare itself is indeed complex with all its specialists addressing the miraculous mechanisms of life, but healthcare administration is not about the biochemical process through which thought, for example, is sustained in our cerebellum. It’s a framework for: a) providing services, b) getting paid for those services, and c) Keeping costs fair and reasonable.
The problem we address today arises because for the last sixty years that simple framework has been under siege. Healthcare has been a money-making machine for numerous and powerful third-party players who engage in a game of politics and cat and mouse with government and experts and you and I—a game whose twists and turns have created a labyrinthian world indecipherable to the average American and infinitely more complicated than the actual problem it purportedly seeks to solve.
In a world where mathematical algorithms can formularize any image and computers can untangle the mysteries of DNA, surely we don't need a million people to help us pay our doctors.
HEALTHIER HEALTHCARE maintains, therefore, that the only way to rectify this is to focus on the fundamental purpose of healthcare—a healthy citizenry at reasonable cost—and to build an optimal solution from today's possibilities. To accomplish this, HEALTHIER HEALTHCARE eliminates the administrative roles of both government and big business and hands control back to the primary participants by shifting the overall dynamic from one of hierarchical action and consequence to one of cellular action and consequence which relies on the following elements:
The patients
The providers
The internet
An investment fund owned principally by the patients and which is generated primarily through patient premium payment/investment but which can also include provider investment, government investment, as well as general investment. This fund guarantees an attractive and secure minimum annual return to all investors including the patients.
Software supporting:
An interactive screen dialogue for the patient involving choices and consequences.
An interactive screen dialogue for the provider involving choices and consequences.
A mathematical algorithm which dynamically modulates the consequences of patient and provider choices in such a way as to guarantee at least the minimum return for the fund.
Databases containing all information pertinent to the operation of the software as well as access to relevant outside databases as needed and authorized (financial institutions, government statistics, payroll records, etc.)
Though there are many benefits which will be explored later, participants can choose to interact at a minimum level. Patients, for example will minimally use the software to:
Locate, contact and engage providers based on judgement factors provided by the software, and upon the level of financial responsibility they wish to incur
The Providers will minimally use the software to:
Review their own judgement factors relative to competitors
Price their products/services relative to the mean/average cost of similar product/services in their areas.
Record and bill their product/services
Because the patient/provider dynamic will no longer be beholden to the needs of third parties, the vast majority of bureaucratic requirements can be eliminated. For the patients here will be no forms, no checks, no meetings, no battles with insurance companies. Their only human dialogue and ultimate physical connection will be, as it should be, with their chosen provider(s). Their own choices will determine the financial implications for them.
For the providers there will be no government or mega-company interference in their administrative activities. They will set their own rates and decide what products and services to use, and what hospitals, clinics or partnerships and alliances are appropriate for them. Their current mountain of bureaucratic requirements will be reduced to the mere entry of the treatments they have executed in the context of their overall choices. The consequent financial and other implications will ripple transparently though the system, much as the implications of check-writing ripple throughout any good business support software, and their own choices will determine the ultimate financial implications for them.
The result of this simplification will be a healthcare dynamic that is so efficient and complete that it won't even seem to exist. It is a dynamic whose simplicity allows it to serve the needs of the true participants by capitalizing on its own vast resources to support them. It will transparently and continuously analyze ongoing healthcare transactions, diagnosis, results, costs, conflicts, etc. in order to detect patterns of success and failure—of efficiency and abuse—of conflict and resolution—of weakness and strength, and then boil it all down to simple and straightforward implications which will be organized and available to all of us as appropriate in our own individual context and thus guide us and inform us and protect us from abuse and confusion and help us make the best decisions—and incidentally help nip potential legal conflict in the bud.
It’s also a dynamic which replaces upward spiraling political cost-control with an ancient and dependable downward spiraling cost-control re-enabled through creative use of powerful technologies.
"But how on earth could you get such a system past Power and Politics?" you ask.
"That's the big issue isn't it." I reply, "But it is possible if we design it like a seed, and plant it in some forgotten corner of society and wait for it to grow like an oak and gradually reveal its strength and simplicity.
"It is a dynamic whose time has come," I continue, "and which with careful planning can be implemented with minimum trauma to society itself."
"IMPOSSIBLE!" You say.
Read on!
H E A L T H I E R H E A L T H C A R E
The Problem
Fifty-odd years ago, as a young man working a summer job, I sliced off the end of my left index finger and suffered the small death as it fell, slow motion, into the rubble next to the saw. I grabbed the strangely foreign but still living digit, and raced ten minutes to the nearest hospital where I waited four hours for administrators to decide who would take financial responsibility. It was my first encounter with our healthcare bureaucracy.
The finger died.
The problems even then were unnecessary complexity, cost beyond individual reach, and a mix of third party players that blurred the line of responsibility to me, the patient. Are the problems today any different? Have we made any real healthcare headway during the last fifty years, or just added more layers of functional and regulatory complexity to a healthcare house of cards?
The answer to that question is obvious to all, and yet as a nation we have been perennially incapable of looking the problem in the eye and taking effective action. Each time there has been a real opportunity for positive change we have assigned politics and power to the task of renovation with utterly predictable results.
And now we are about to do it all over again!
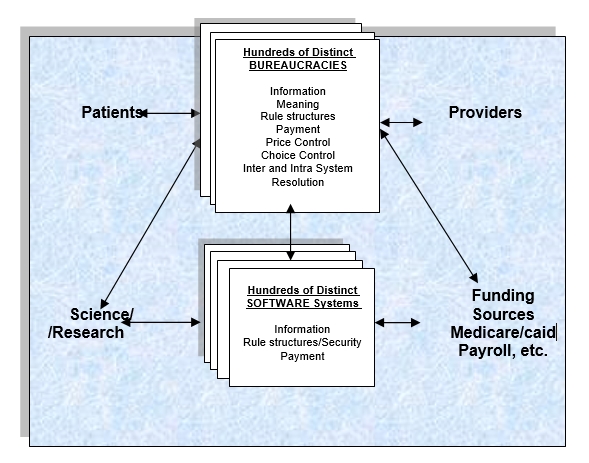
OUR PRESENT PARADIGM
At the core of our current healthcare dynamic is the very useful and attractive concept of shared risk, both public and private. In one way or another, the end users invest a small amount now to create a pool of shared capital to help them avoid a severe financial hit later.
It is the control of this pool of shared Capital which originally created the need for a bureaucracy which was not part of the original patient/physician relationship. Over time, this money-controlling bureaucracy, whether public or private, has gradually come to dominate the healthcare transaction and in the process has distorted the primary purpose of the system, clouding understanding, motivation, and consequence for patients, physicians, providers, and the public at large.
WHAT IS
Many think that administrative inefficiency within this structure is the key contributor to healthcare cost, but real culprit is the existing paradigm itself, which by handing cost control over to a bureaucracy which doesn't feel the edge of consequence, guarantees a cost creep which ripples through the entire bloated structure making it the most expensive in the world.
These top-down methods also add greatly to the complexity of our current healthcare system which opens the door to corruption and inefficiency which extends even to the programming code itself,
The situation obviously demands dramatic change but we must remember that our solution cannot sacrifice the excellence which has characterized the best in this current system—the development of the best equipment, medicines, and professionals in the world.
So our new dynamic must use clarity and simplicity to eliminate the negatives of the old, but to retain its positives, and to do even better by streamlining and encouraging new opportunities for research and new opportunities for preventive healthcare in particular.
We must also recognize that the implementation of our solution cannot be sudden We must plant the seed, not the tree itself, and allow time and Shakespeare´s broils (to) root out the work of masonry so that new vitality may gradually replace decline and give wise design and technological excellence time to unravel entropy´s death-grip on our nation's healthcare system.
The Solution
HEALTHIER HEALTHCARE uses technology to replace bureaucracy by replacing our current hierarchical top-down control of events, costs and conflicts, with bottom-up cellular control of all activity including the control of the Fund itself. The integrity of this process will be protected with sophisticated software which incorporates an underlying dynamic for cost control designed to reverse cost creep.
This shift from top-down to bottom-up cellular control is a paradigm-shift that is difficult to grasp for most of us—and difficult to accept for the guardians of our current dynamic because it requires that they do the thing they most fear—relinquish control of our healthcare process to the participants themselves.
So to understand how such a shift could work in our nation's favor—and why—consider for a moment an analogy involving Michelangelo’s statue of David—a magnificent accomplishment by a human god, embodying both the beauty of the human form and the power of the human spirit. With great skill Michelangelo carved his vision with chisel and hammer from solid rock—and of course all of us admire the amazing ability and method of this great artist.
But nature used an almost opposite method in order to bestow on the original David, that most complicated and flexible of all known structures—life itself—and the difference in these methods of creation mirror the relationship between yesterday’s healthcare and tomorrow’s.
The shape of living beings is not determined from the outside impact of chisels but from the inside impact of genetic structures. No unseen hand carves the trunk of the elephant, its shape being rather the consequence of trillions of minute and seemingly unrelated biochemical decisions based on immutable laws of matter, biology, and electricity and guided and governed by the particular molecular structure of DNA contained in the fertilized egg - a biochemical reaction leading to another and another and another whose twists and turns and variations all depend on that DNA.
All of the decisions begin at the molecular or cellular level, and order is imposed not from above, but from below, and in this remarkable and almost perfect process there is no managing entity.
And the miracle doesn't end there, because the resultant creature is not static but flexible, it is capable of dealing with change and the vast numbers of variables that surround it. In this it acts as a unit whose various components are in perfect harmony and ready to support the whole.
This dynamic is so reliable that all life depends utterly upon it, but it is certainly not the dynamic underlying our crippled healthcare system.
That dynamic was conceived and constructed, as was Michelangelo’s statue, from the top down. The tools and structures were designed to control the outcome as it emerges from the clay of humanity itself. Government agencies control and oversee all Medicare and Medicaid healthcare transactions. Insurance companies react to events with countermeasures and formulas. Legal referees interpret conflict according to legal structures imposed over all. The patients and the doctors are constrained by this web of structures imposed from above and the outcomes are determined by the actions of society's chisel.
But as time passes and society changes, levels of complexity within this dynamic surge and its inter-dependencies proliferate, and it begins to demand greater flexibility and unity than that afforded by the institutions and entities that support it—and now it begins to decay.
We see its limitations as one mega-player learns to game the other for advantage and is later gamed upon in an endless battle involving all of us and whose complexity grows exponentially and whose only real loser is society itself. This socio-economic rise-and-fall dynamic which now confronts us in the healthcare crisis is really just another instance of the dynamic that has played out in human society for thousands of years,
WHAT COULD BE
But now for the first time in history sophisticated technology can reliably allow us to harness nature’s bottom-up solution, at least for healthcare, and thereby return complete control to the tens of millions of patients and providers themselves.
In this HEALTHIER HEALTHCARE dynamic the patient/provider relationship, not bureaucracy, will provide the governor for balanced and straightforward cost control. In this cellular framework, the patient’s intimate need for a fair price will create a healthy and necessary tension with the physician’s intimate need for a fair profit which will damp cost inflation at its immediate source and prevent the system from spiraling out of control.
But what does this framework look like and how exactly can if be both effective and incorruptible?
HEALTHIER HEALTHCARE achieves its strength and integrity by adhering to three basic principles:
First - the framework needs to attach significant consequence to the choices of both the patient and the provider.
Second - both the patient and provider interface with the software must be exquisitely simple and crystal clear.
Third - the overall integrity and security of the system must be transparent and above reproach. It cannot be guaranteed from the top down as is currently the case but must recognize its own problems and solve them through mechanisms which tap into the self-interests of the millions of participants themselves.
What would this system look like?
The Software
The engine of this approach to healthcare administration is almost pure software. That software must be designed by creative minds but built with the collaboration of the best of established experts. These two mindsets in combination will guarantee the excellence of the end-product and be responsible for its ongoing maintenance.
The internet will provide the common ground for all participants, a common ground that uses very few screens and is utterly transparent and simple in the way that Google is simple. Those who don’t possess computer knowledge or computers can work with friends or family members who do and/or gain computer access at one of the many available internet cafes or Public Libraries. At least initially, public training should be available, though if we can achieve Googlesque simplicity the learning curve will be short.
The lifeblood of the software will be an impartial rule structure imbedded like DNA in the programming code with highly automated and secure processing which delivers to the patients and providers all the information necessary for decision-making in a clear and simple manner.
Also contained within the software will be algorithms for consequence, interface to government/private funding and the capacity to access tax, payroll, benefits, etc., and private banking systems as needed and authorized for money transfer.
Parallel functions and processes will guarantee accounting integrity as well as security and privacy and fai-lsafe capacities, but such processes are nothing new. Every bank employs them now and they are omnipresent in our plastic society—but as we shall see, in this case we can do even better because the very nature of our unified and integrated, and clarified system opens the door to other powerful guarantors of integrity—the participants themselves who will automatically be notified when any activity that might affect them wanders too far from accepted norms.
These kinds of capacities underscore the absolute need for a participant interface of maximum clarity and simplicity, and to accomplish this, beside inspired use of our great technology, other design considerations are important.
The current healthcare structure, for instance, reflects too much the needs of the exception and the potential for conflict. Patients inside the structure are often confronted by issues that are confusing and complex—and irrelevant in most cases. Our central design should be shaped instead by the predictable non-confrontational needs of the vast majority of participants.
Exceptions and conflict must therefore be walled off from mainstream processing and dealt with in a separate world so that the related logic and the details will not influence mainstream design and not be visible to the average participant who will never be unnecessarily exposed to them directly or indirectly.
Of course with use, the software will evolve to reflect changing times and technologies and opportunities but these will be much easier to implement when built on this clear and integrated base.
THE PATIENT INTERFACE
For typical patients, the Patient Resource Screen along with several simple subordinate-screens, will provide their only interaction with healthcare administration. From that screen they may access any information relevant to their healthcare needs including the impact, if any, on their financial circumstances. There will be no forms no checks no meetings no premiums, no battles with insurance companies. The only human dialogue and ultimate physical connection with the healthcare system will be, as it should be, with their chosen provider(s) with whom they will also be able to communicate easily via their MY PROVIDERS option.
The screen will enable patients, with the help of their families or legal representatives if necessary, to choose their providers based on clear, simple, and instantly available criteria.
But how?
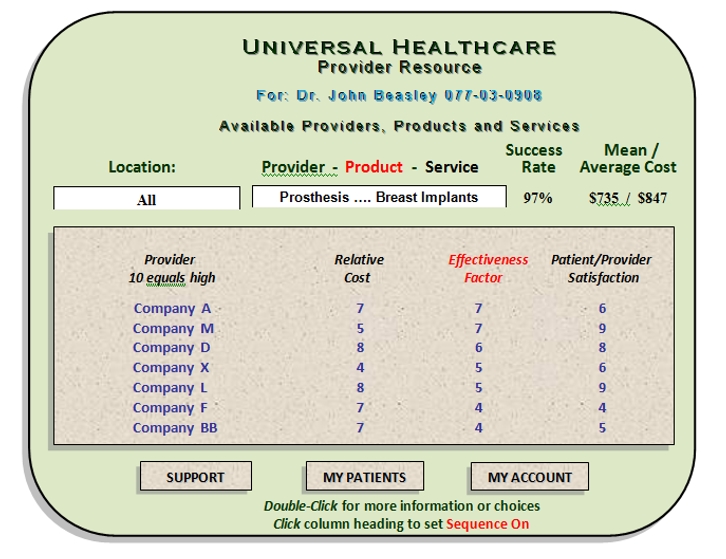
Most of us have always looked for help in choosing a physician by asking family, friends and associates the following questions regarding potential healthcare providers: How effective are they—how satisfied are our friends—how much does it cost?
The unified nature of our system allows us to provide answers to those very questions but the information is likely to be far more accurate and fair than the information generated by any word-of-mouth rumor mill. Our software will distill those answers from millions of actual transactions and activities within and without the system itself so that it becomes clear and simple and available to the primary healthcare players. In our system that distilled information is presented in the form of the following Judgment Factors which are presented on a 1 to 10 value scale, 10 being best:
Relative Effectiveness
Patient Satisfaction
Relative Cost.
Particularly important to the patient is the Relative Cost factor which drives the financial consequence of their choices. Patients can opt for little or no personal financial consequence (beyond their basic support for the shared fund) by choosing the lowest cost provider available.
But patients can alternatively decide to contribute their personal funds to the cost of their own healthcare by choosing one of the more expensive providers, potentially with higher Relative Effectiveness or Patient Satisfaction factor ratings. In that case a set of payment options depending on the precise nature of the patient’s financial circumstance would be listed on the screen.
Their choice might impact their paycheck deductions, their bank accounts, their credit cards, their future taxes, future benefits, or their estates, or their public support. In some cases it might even involve family members or friends who might be provided with incentives to cooperate.
Ongoing detailed information regarding the impact of their choices on their financial positions will be available to them at any time via their MY ACCOUNT option.
Finally, the SUPPORT option on the Patient Resource Screen will provide shortcuts to the vast array of information on the web related to their specific infirmity. It can also include access to support groups made up of others with the same ailment, or to an array of preventative alternatives and what-if scenarios tailored to that patient.
THE PROVIDER INTERFACE
Provider investigates sources and prices for goods and services that he needs
Without government or mega-company interference, you as a provider can set your own rates, and decide what products and services to use, and what hospitals, clinics or partnerships and alliances are appropriate for you.
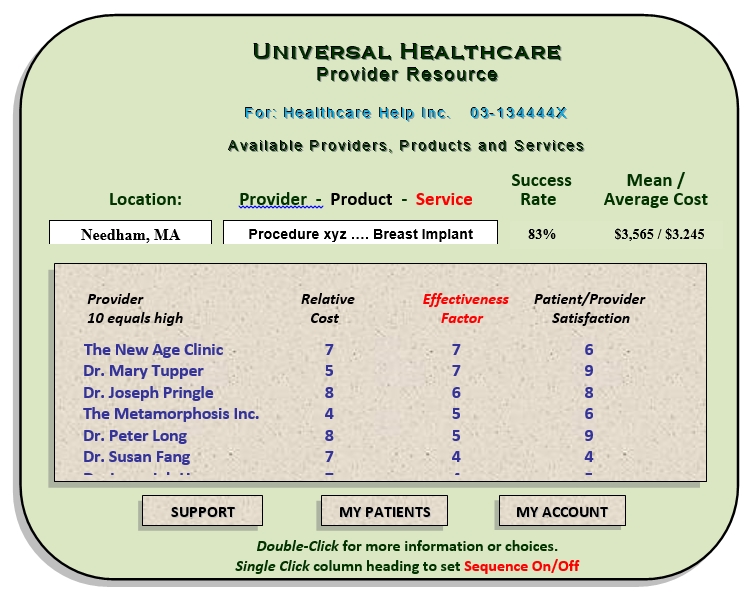
You can determine how your choices fit into the whole by accessing the Provider Resource Screen which represents your window into universal healthcare. In the first example a Dr. Beasley investigates sources, prices, and success rates for silicon breast implants.
These screens will provide information on prevailing rates and ratings for all providers and healthcare goods and services processed within the system as determined from actual billings and results. These include average and mean costs for specified areas/products/ services.
Provider uses Resource Screen to price his own services
In the second example the clinic Healthcare Help Inc. uses the Provider Resource Screen to look at the competition in order to position their own rates for specific goods and services.
The providers can bill what they want and be paid, but they will be placed in the corresponding cost category which may shift the cost over to future potential patients who will make their decisions accordingly.
Providers will bill HEALTHIER HEALTHCARE online and receive payment automatically and electronically from the shared fund (see below), and they can determine via their Provider Resource Screen how well they are doing, not just financially, but professionally relative to their peers.
***
That´s HEALTHIER HEALTHCARE for most of us—somewhat oversimplified in summary, but the heart of what is actually necessary. Software, not bureaucracy, will take care of all the administrative needs of almost all participants. Cost control will be managed, not by bureaucracy, but by cellular consequence and incentives and disincentives for every action and for every participant.
Decisions will be immediate to the action and to the participants, and less susceptible to the corruption that grows in more complex and layered structures. The net effect over time should be dramatically lowered healthcare cost—even the likelihood that efficient universal healthcare for every citizen of our nation might cost less than our current bloated system.
Only with conflict or anomalies outside the vast array of predictable situations will it become necessary to enter the next level of complexity - but this in itself is not yet excuse enough for bureaucracy.
Conflicts and Exceptions
Conflicts and exceptions, which will inevitably occur within any healthcare system, always add complexity. In this case these will be dealt with by a separate branch of the software itself.
Carefully structured conflict and exception Resolution Opportunities between provider/patient and provider/provider will take advantage of the transparency and ease of access to pertinent information and global patterns. These will take the form of electronic dialogues between the participants (or their representatives) whose goal is confirmation of an agreement by all parties.
But even before this point is reached, transparency itself can be expected to diminish the likelihood of confusion or open conflict. All parties will be apprized by the software if any ongoing relationship or event departs significantly from either financial or medical norms, and will be encouraged via reminders to keep an open dialogue to try to nip any problem in the bud. The system will also automatically offer parallel situations and resolutions to help clarify the nature of any problem.
Only if significant conflict resolution efforts by both sides result in failure will the software initiate an electronic dialogue involving an independent conflict resolution specialist or healthcare expert. If that fails the parties can then leave the confines of the healthcare structure itself and access the courts at their own expense.
But in order to minimize these outside-the-system conflicts in the future, such unresolved anomalies will be forwarded to a small team consisting of healthcare experts and software professionals whose goal will be to understand the anomaly and incorporate its resolution into the software for reference and resolution by future participants.
Note that as long as conflict resides within the healthcare structure itself, resolution is in the hands of the primary participants and not third parties. These are the individuals closest to the problem and most capable of resolving it rapidly if given a chance. Only if they are unable to solve the problem themselves is it given to a conflict resolution expert, and then any resulting resolution is forwarded to an action team responsible for updating and maintaining the software so that in the future similar problems can more likely be handled automatically.
PROVIDER ABUSE
Like the sleuth software which I developed for Medicare in the early 1990s, sophisticated analysis within the software will constantly scan for suspicious or aberrant patterns and analyze electronically-entered patient and provider feedback which may suggest manipulation of the system. It will issue warnings, first to the suspect party, then if the pattern continues, to all involved parties, and finally as a last resort as a flag to the general population via the Patient Resource and/or Provider Resource screens. As mentioned above, the participants will have recourse to a rigorous online dialogue designed to resolve conflict and correct the record if necessary. With evidence clear and available to all, many errors or disputes can likely be solved without involving third parties.
The negative implications of non-resolution are obvious but such resolution might even be positively incentivized in order to reduce the need for human intervention and thus the overall cost of healthcare. Well defined temporary discounts might be offered to participants as a reward for swift resolution.
PATIENT ABUSE
Patient abuse will most likely take the form of overuse. If that overuse becomes serious as measured against parallel usage within the system, patients and relevant providers will be warned that they have departed from acceptable norms and encouraged to justify their actions or move toward more reasonable behavior. The patient will also be informed of escalating financial consequences if the pattern continues without justification.
Funding
At this moment, the funding of healthcare is fragmented with hundreds of insurance companies, and government agencies, and clinics and hospitals and foundations and welfare organizations and many mechanisms footing the bills for the indigent and the poor and passing those cost indirectly on to us – increased premiums, increased taxes, higher hospital bills etc.
So the idea that we don’t want a universal system because we don’t want to pay for it is inaccurate and unrealistic. We are paying for universal healthcare already, however indirectly, and we are paying much more than necessary because the whole is disorganized and redundant and messy. A properly organized comprehensive solution would be inherently less expensive and provide a framework in which additional opportunities could be exploited to make it even less expensive.
Whether our new system is public or private and whether our central fund is generated by tax deductions or by premium payments or investment opportunity, it will be defined and generated in such a way that its very structure contributes to cost control and encourages responsible action by the participants.
There will be two factors which will allow the fund to exert gentle downward pressure on healthcare cost:
Ownership - The fund must be clearly our fund (doctors and patients), not the fund of someone else who needs to milk it for profit, and
Return on investment - The fund will be treated like an investment fund for the participants with returns tied to overall healthcare performance.
The system cost formulations will be tuned to yield an average of say 10% for all investors (ourselves) but the formulations will be based on overall healthcare expenditure targets which will vary from year to year based on prior year performance and designed to foster in the participants a communal attitude which favors the efficient operation of the system in general.
If annual costs fall below target (which they should do initially with lowering costs), return on investment would grow above 10%. If annual costs exceed that target, return on investment would shrink.
Patients will participate via their monthly premiums (or if public, through payment of a healthcare tax).
Providers will participate via voluntary investment or through the imposition of an annual fee which licenses participation in the system.
Security and Financial Integrity
The engine of this approach to healthcare is almost pure software. That software must be built with the collaboration of experts, but designed by innovative minds unattached to convention. In combination these two mindsets will guarantee the excellence of the end product and form the foundation of a team responsible for ongoing maintenance.´
The integrity of the whole must be above reproach. The integrity of existing software driving far more complex paradigms and involving great sums of money has evolved for decades and the necessary technological structures for security, integrity, and failsafe are easily available today. But HEALTHIER HEALTHCARE provides a whole other level of integrity because its paradigm will guarantee a level of transparency that gives every participant the ability to see the details and the implications of activity.
This means that at a cellular level millions of participants will be zealously guarding the integrity of their own transactions as they see the consequence of their actions and the actions of others trickle down to their pocketbooks. Any finagling by a provider or other participant that impacts bottom lines will be evident and objectionable.
To help give individual participants the sense that they can rely on the system, the same level of sophisticated analysis used to evaluate physician success rates should be used to flag financial activities which depart from norms calculated by the system itself. The cost factors, for example, which contributed to the patient´s original decision to go with a specific physician, can be compared to subsequent results for that patient and flagged for him if out of line.
Tolerance margins for anomalies can be dynamically adjusted to levels which reduce the numbers of false positives.
Another guarantee of system and financial integrity will be simple barometric information produced on a daily basis to be reviewed by statisticians and available to all other participants as well. The indicators will distill the results of sophisticated internal analysis analogous to that which guarantees processing integrity every time you turn on your computer. Anomalies will be flagged as necessary.
The task of creating this internal analysis will be entrusted to accountants/scientists familiar with the latest techniques in statistical analysis. The corresponding software will be updated on an ongoing basis much as virus protection software is updated to counter evolving strains.
The integrity of the software driving the whole must be above reproach. The integrity of existing software driving far more complex paradigms and involving great sums of money has evolved for decades and the necessary technological structures for security, integrity, and failsafe are easily available today.
But our paradigm will add to these existing structures a level of transparency that gives every participant the ability to see the details and the meaning of suspicious activity At a cellular level millions of participants will be jealously guarding the integrity of their own transactions as they see the consequence of their actions and the actions of others trickle down to their pocketbooks.
And to help give individual participants the sense that they can rely on the system in general, the same level of sophisticated analysis used to evaluate physician success rates might be used to flag financial activities which depart from norms calculated by the system itself. The cost factors, for example, which contributed to the patient´s original decision to go with a specific physician, can be compared to the results for that specific patient and flagged for him if out of line.
All anomalies which exceed tolerance levels will be flagged for the participants and tolerance margins will be dynamically adjusted to levels which reduce the numbers of false positives.
Another level of financial integrity will be established for the system in general with simple but key barometric information produced and reviewed by statisticians on a daily basis. The information, which would be available to all other participants as well, will serve a function similar to that of the indicators on your automobile´s dash which allow you to know that your vehicle is functioning properly, but in this case the indicators will distill the results of sophisticated internal analysis analogous to that which occurs every time you turn on your computer and wait while software confirms the viability of its operating system.
The task of creating these barometric indicators will be entrusted to scientists familiar with the latest techniques in statistical analysis and the software they create to accomplish this will review all pertinent information on an ongoing basis just as virus protection software reviews your laptop internals to counter hacking.
The Rewards of Unity and Simplicity
For science, preventive medicine, healthy diet, patient peer group support, emergency response, the issuance of critical flags and notifications, and fundamental healthcare itself, the unity and accessibility of information and trends afforded by our simplified structure will yield untold benefits.
Science can use its easy access to our system to enhance our nation´s level of healthcare excellence.
Pharmaceutical integrity will benefit greatly from the presence of uniform information and ease of access to trillions of transactions. And it can also benefit from the capacity for rapid deployment of results and warnings when necessary. In an instant, defective medicine alerts can appear on millions of provider and patient screen.
Patients will have everything they need in physician support, and important information regarding diet, and support groups, etc. calibrated to their specific infirmity, just a click away.
And all of this adds up to a healthier more productive citizenry…
…and a healthier and more competitive nation.